Diminished Ovarian Reserve
Diminished ovarian reserve at a glance
- Diminished ovarian reserve (DOR) is a condition in which a woman’s ovaries contain few eggs and/or eggs of poor quality, causing infertility in women or making conception more difficult.
- Women with diminished ovarian reserve were either born with fewer eggs than average, lose them faster than average or over time the eggs accumulated more damage than is average.
- Smoking, genetic abnormalities, cancer treatments with radiation and certain chemotherapy agents, possibly environmental toxins, as well as the surgical removal of part or all of an ovary can negatively affect a woman’s ovarian reserve.
- By measuring a women’s ovarian reserve (the number and quality of eggs in her ovaries), a physician can determine if the ovaries demonstrate accelerated aging, and can better predict diminished fertility and pregnancy outcomes with in vitro fertilization (IVF).
- Ovulation problems are one of the most common causes of infertility.
- The primary ways to measure ovarian reserve are antral follicle counts, estradiol levels, clomiphene citrate challenge, anti-Müllerian hormone (AMH) levels, follicle-stimulating hormone (FSH) levels and estradiol levels.
What is diminished ovarian reserve & how is it a cause of infertility in women?
Ovarian reserve refers to the number and quality of eggs a woman has in her ovaries. Women with diminished ovarian reserve either have few eggs remaining or eggs that are of poor quality. This can be a cause of infertility. Women with diminished ovarian reserve can also have a reduced chance of conceiving with in vitro fertilization (IVF) and other fertility treatments. They also have a higher chance of miscarriage.
In practical terms, ovarian reserve is the same thing as the biological clock. Most women are aware that there is such thing as a biological clock, but they are frequently uncertain when this clock really begins to tick. Some women remain fertile into their late 40s, while other women lose their fertility in their 20s and 30s.
Many cases of diminished ovarian reserve are never explained, according to the American Society for Reproductive Medicine, but common causes are:
- Age > 35.
- Smoking.
- Genetic abnormalities (Fragile X premutation or X chromosome abnormality).
- Cancer treatments with radiation and certain chemotherapy agents.
- Surgical removal of part or all of an ovary.
Is low ovarian reserve increasing and is it happening at earlier ages?
The incidence of low ovarian reserve (diminished ovarian reserve) seen in fertility clinics has been increasing. A general reason is that maternal age at first pregnancy is higher these days than with previous generations. This can be due to women putting off having children while engaged in their careers and for a variety of other reasons. It results in more women trying to conceive after their prime age for conception.
This trend is evident in the increase in age-related infertility and the subsequent increase in assisted reproductive technology (ART) such as IVF to overcome it. According to a Fertility and Sterility evaluation of women undergoing ART from 2004 to 2011, the prevalence of DOR increased from 19% to 26%. The good news is that the incidence of poor ovarian response to stimulation decreased and the live birth rate increased in the group studied.
At the same time, we are seeing more women of a younger age with DOR than previously. This is anecdotal at this time, and more research is needed to clinically verify that an increase of DOR at younger ages is occurring, as well as the reasons behind it.
Role of endocrine disruptors in DOR
One possibility is that environmental toxins could be causing a higher level of damage to female eggs. These toxins can affect hormones and female eggs. Phthalates, which are chemicals in plastics, work as endocrine disrupters. Endocrine disruptors like phthalates and others can block connections between the female sex hormones estrogen and their receptors, changing the function of the hormone system. They similarly affect male testosterone.
Dr. Murray’s detailed blog, with tips on disrupting the disruptors
Endocrine disruptors are linked to unhealthy impacts on eggs and sperm. Bisphenol A (BPA) changes endocrine pathways affecting reproductive health and compromises embryo implantation. Endocrine disruptors are suspected to change the germ cells that later develop into eggs and sperm cells.
Women who are employed in certain types of work, such as dental assistants, industrial and agricultural workers, and hair stylists, may be at risk of exposure to ovarian reserve harming toxins.
When to seek ovarian reserve testing
The following people should see a fertility specialist for ovarian reserve testing.
- Women who are older than 35 and have not gotten pregnant after six months of unprotected, frequent intercourse should be tested for ovarian reserve.
- Women not getting pregnant who have experienced one of the causes of DOR listed above (genetic abnormalities, smoking, etc.).
- Those having trouble conceiving who have symptoms of primary ovarian insufficiency that are hot flashes, vaginal dryness and irregular periods.
Don’t delay DOR testing
With DOR increasing and occurring in younger women, it is more important than ever to seek testing as soon as you suspect your reserve may be depleting.
Request an Appointment
Why does infertility in women happen sooner for some than for others?
Every woman is born with all the eggs that she will ever have: approximately 2 million. Every day, including through childhood, women lose eggs. Eggs are lost even if a woman is on birth control, is pregnant or has infrequent menstrual cycles.
Additionally, as a woman ages, the eggs and the cells around them can accumulate damage that is never repaired. Therefore, as a woman ages, not only does she have fewer eggs, but a higher percentage of her eggs are abnormal due to damage from the aging process.
If she ovulates an abnormal egg, her chances of pregnancy are lower, and her chances of miscarriage and having a baby with an abnormality are higher.
Women with diminished ovarian reserve were either born with fewer eggs than is normal, lost them faster than most women, or over time the eggs accumulated more damage than normal.
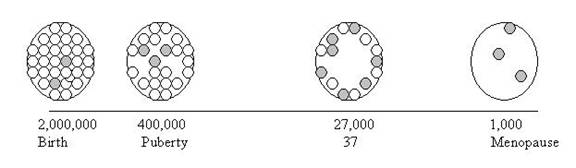
The picture above illustrates the phenomena of egg depletion over time. The white circles represent normal eggs and the grey circles represent abnormal or damaged eggs. Notice that at birth, when egg number is at a maximum, there are a minimum number of abnormal eggs.
At the onset of puberty, a woman has already lost approximately 75% of the eggs she was born with. By her late 30s, a woman’s egg numbers continue to decline and notice in the illustration that now the ratio of normal to abnormal eggs has shifted, with a much higher proportion of abnormal eggs. By the time a woman reaches menopause, almost all remaining eggs are abnormal.
What is ovarian reserve testing?
Ovarian reserve testing measures the number and quality of eggs a woman has in her ovaries. With ovarian reserve testing, the physician can estimate whether a woman’s eggs have the fertility potential of most women her age, or if her ovaries demonstrate accelerated aging.
A woman’s diminished fertility potential is predicted by any abnormal ovarian reserve test. This means that while repeating the test may yield a normal result, any prior abnormal result predicts significant difficulty conceiving either spontaneously or with aggressive treatments including IVF.
However, it is very important to understand that even a significantly abnormal test result cannot exclude the possibility of pregnancy. Ovarian reserve testing best predicts pregnancy outcomes with IVF.
Brenda wouldn’t let diminished ovarian reserve stand in her way, so she found TRM and put her faith in Dr. Murray.
Brenda’s Story
Types of ovarian reserve testing for possible infertility in women
Antral follicle count
We typically perform this test on the third day of a woman’s menstrual cycle and use a vaginal ultrasound to measure how many follicles she has in a given month. A follicle is a collection of cells that contains the egg and nurtures the egg as it develops.
If the follicle survives to a certain size, it begins to collect fluid around the egg. This fluid is visible on ultrasound and looks like a small black circle on the ovary.
If doctors see a large number of follicles, this indicates that the ovary has an ample number of eggs still in hibernation. If they see few follicles, this means that the ovary has a minimal number of eggs.
How antral follicle count tests are performed
- On the same day that a patient’s FSH and estrogen levels are measured, she will have a vaginal ultrasound.
- The physician will count the number of follicles on each ovary.
- If fewer than 10 follicles are seen (on both ovaries combined), a woman is deemed to have diminished ovarian reserve.


Anti-Müllerian hormone test
Anti-Müllerian hormone (AMH) is a hormone delivered by the antral follicles. Each follicle emerging from the storage pool secretes a small amount of AMH. The more follicles emerging from storage, the higher the AMH level. As a woman ages and the number of her eggs naturally decreases, so does her AMH level.
While low levels of AMH are an indicator for diminished ovarian reserve, higher than normal levels of AMH can reveal polycystic ovary syndrome, which can also affect a woman’s fertility.
AMH levels can be measured at any point during a woman’s menstrual cycle. AMH is a fairly accurate tool used to predict how many eggs we can induce to grow during a treatment cycle.
Clomiphene citrate challenge test (CCCT)
Some women have normal labs on the third day of their menstrual cycle but still have diminished ovarian reserve. The clomiphene (Clomid) citrate challenge test (CCCT) detects about 10% more cases of diminished ovarian reserve than with labs alone.
How the test works:
- The CCCT is based on the premise that a woman with normal ovarian function should respond to fertility drugs.
- We obtain labs on the third day of a woman’s menstrual cycle, and then the she takes 100 mg of clomiphene citrate daily for five days.
- Clomiphene citrate temporarily raises FSH, stimulating egg development and estrogen production.
- One or two days after finishing the clomiphene citrate, we repeat the labs to obtain a second FSH reading.
- FSH levels less than 10 mIU/ml are considered normal.
- Levels from 10-15 mIU/ml are considered mildly elevated and abnormal.
- Levels greater than 15 mIU/ml are significantly elevated.
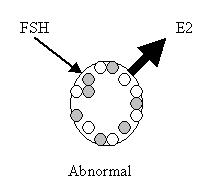
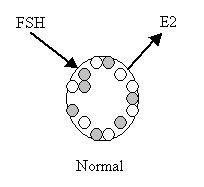
A woman with normal ovarian function will produce a lot of estrogen and inhibin (another hormone) in response to clomiphene, which will cause her FSH to decrease to normal levels.
A woman with poor ovarian reserve will not respond to the clomiphene citrate as well and will not have increased estrogen and inhibin production. In this case, the FSH will stay high.
If the woman has an elevated FSH or estrogen results on the initial labs that were drawn on the third day of her menstrual cycle, or a high FSH after the CCCT, then she has diminished ovarian reserve.
Estrogen levels are not measured again on the post CCCT labs, because unlike the estrogen level on day three of her menstrual cycle, the labs post CCCT, (which is day 10 of a woman’s menstrual cycle) are not predictive of fertility potential.
Follicle-stimulating hormone (FSH) & estradiol infertility test for women
Baseline hormone evaluation of FSH and estrogen level is the most common test of ovarian reserve.
How the test is performed
- Using the first day of a woman’s menstrual cycle as day one, a woman ideally comes to the clinic on the third day of her cycle, (or alternatively, days two or four) to have her FSH and estrogen levels measured.
- An abnormal test is an indication that the ovarian reserve is diminished.
- An FSH > 10 mIU/ml or an estrogen > 75 pg/ml are considered abnormal.
If the test results are abnormal, the physician will have to put this result into context, considering the patient’s entire evaluation.
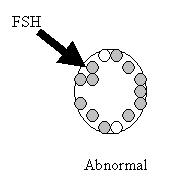
If the ovary is working well, it should not require a lot of FSH to function. If the FSH is high, the ovary probably isn’t working efficiently and the patient has diminished ovarian reserve.
The estrogen (estradiol) level is important for several reasons. For the sake of simplicity, think of estrogen as a way to validate the FSH level.
A high estrogen level will lower the FSH and bring an abnormally high FSH into the normal range. Therefore, if both FSH and estrogen are in the normal range, this is reassuring.
Why we don’t recommend home tests for ovarian reserve
There is now a commercially available kit that allows a woman to measure her FSH level at home. The kit measures the amount of FSH in the urine and can reliably tell her if her FSH is > 10 mIU/ml.
We do not recommend this test. First, the test is fairly expensive. Second, and more importantly, this is only helpful if it is abnormal.
At home tests can provide clues but no definitive answers
Why not to be reassured by a normal result
This urine test does not assess estrogen levels. Because estrogen levels affect FSH levels, an individual has no way of knowing whether a normal test is valid.
Explore your treatment options
Ten couples with the same circumstances may all make very different decisions. IVF, GnRH, eSET, ICSI – there’s an alphabet soup of possible treatments for infertility, but not all are going to be right for you. TRM helps you decide the best approach for your specific situation.


