For OBGYNs: Pregnancy of Unknown Location
Our practice liaison often fields referral questions from OB/GYNs about pregnancy of unknown location (PUL) in their patients. As infertility specialists, we are familiar with problematic embryo implantations, such as ectopic pregnancies or pregnancies in the wrong part of the uterus. Also, OB/GYNs often need to refer these patients to us, as a PUL may indicate a fertility issue we can treat.
We hope the following information on PUL will be of help to OB/GYNs.
Expert Treatment. Total Commitment. TRM.

At Tennessee Reproductive Medicine, you’ll find a team of professionals dedicated to delivering the highest quality of compassionate fertility care.
Request an AppointmentClinical approach to intrauterine pregnancy & ectopic pregnancy PULS
A pregnancy of unknown location occurs when a woman has a positive pregnancy test but no signs of the two types of PULS, intrauterine pregnancy (IUP) and ectopic pregnancy (EP), are found on transvaginal ultrasound. According to the National Institutes of Health, the reported rates of pregnancy of unknown location varies widely from 5-42%.
A PUL is not a diagnosis, but a classification term for this occurrence. Sometimes there is no final diagnosis, and the pregnancy is assumed to spontaneously resolve.
Many women with a pregnancy of unknown location will have abdominal pain and/or vaginal bleeding. A PUL may be indicated by passing of pregnancy tissue from the vagina or other symptoms of pregnancy loss, as can a hemodynamic instability.
The initial ultrasound can come up with four possibilities:
- A true PUL, with no sign of pregnancy anywhere.
- A likely ectopic pregnancy.
- An IUP, which is just too early to make the diagnosis.
- A miscarriage is likely due to conception products in the endometrial cavity.
Most women with a true PUL or an IUP will not need treatment because the pregnancy will not last. These women will have a spontaneous miscarriage or resorb an ectopic pregnancy. Because of this, the location of the pregnancy may never be determined.
OBGYN concerns surrounding PULs
There are issues with both over treating and under treating PULs. If a PUL is identified as ectopic too late, it could become life-threatening for the woman. Resolving a pregnancy of unknown location has the potential to terminate what could have been a viable intrauterine pregnancy.
With this in mind, it is important to provide individualized care for each patient. A woman with risk factors for an ectopic pregnancy, such as experiencing a previous ectopic pregnancy or a previous tubal surgery, may have an increased chance of having a PUL become ectopic.
Close monitoring of human chorionic gonadotropin (hCG) levels and regular ultrasounds may help physicians better understand when to act, or not.
Are you a patient who has experienced an ectopic pregnancy and has questions? Contact us today or schedule an appointment online.
Identifying a pregnancy of unknown location
Using hCG levels
After performing an initial transvaginal ultrasound to view into the uterus and identifying no signs of an intrauterine or extrauterine pregnancy, close monitoring of the woman’s hCG hormone must take place.
When an embryo implants in or outside of the uterus, hCG enters the bloodstream. Testing for hCG identifies if there is a pregnancy, but not its location. At one time, it was thought that hCG levels would double every 48 hours in a normal pregnancy. Data from larger sets of viable pregnancy indicate that, in a normal pregnancy, the hCG level will increase by 50% every 48 hours. The lowest acceptable increase is 35% at 48 hours.
Should the hCG levels fluctuate abnormally, typically considered an increase <35% or decrease, this indicates a nonviable pregnancy (ectopic pregnancy or miscarriage).
At a level of 1,500, nearly all normal pregnancies should have a gestational sac visible on ultrasound. One important caveat is that twin gestations (either spontaneous or from fertility medications) may have higher than expected hCG levels prior to when a gestational sac should or could be seen. Furthermore, a twin gestation can have altered hCG kinetics if one twin is doing well and the other is not. A physician should consider the possibility of twins prior to taking any definitive action to resolve the pregnancy with D&C or methotrexate.
Using progesterone levels
A nonviable pregnancy will have a progesterone of < 5 ng/ml. Assuming a woman ovulated just one egg, a progesterone of > 23 ng/ml is almost always intrauterine.
If a woman took an ovulation medication like Clomid or is taking progesterone, these levels may be elevated and are not as reliable for predictive purposes.
The downside to progesterone measurements is that most women fall somewhere between 5 and 23 ng/ml.
Signs of intrauterine and extrauterine pregnancy
In order to accurately identify a PUL, it is important to be aware of what to look for during both an intrauterine and extrauterine, or ectopic, pregnancy. This will usually determine the final type of PUL classification, which will guide treatment. If it is a true PUL or an IUP, the risk to the patient is low. If it is an EP or a persistent PUL (PPUL) from miscarriage, the patient is in the higher risk category. EPs and PPULs can be managed expectantly, with methotrexate or with laparoscopic surgery.
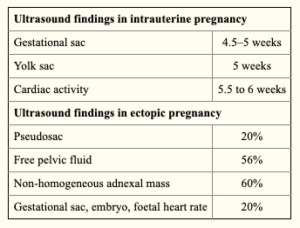
The chart below from the National Institutes of Health relates the indications that should be visible via ultrasound during either form of pregnancy.
In general, a PUL should be managed by watchful waiting until the physician determines the final type of PUL. The woman should be fully informed, in writing, of her risks of having an EP before the final determination of PUL type, so she can be prepared for that possibility.

