Pregnancy Complications
Pregnancy complications at a glance
- Pregnancy complications can arise even in the healthiest of women.
- Common problems in pregnancy tend to include gestational diabetes, preeclampsia, anemia, depression or bleeding during pregnancy.
- If at any time a pregnant woman feels pain, experiences bleeding or senses anything out of the ordinary, she should call her doctor immediately.
- Ongoing prenatal visits to a healthcare provider can help identify potential pregnancy problems early enough to manage the safety of the mother and developing child.
Why do pregnancy complications occur?
It is normal for pregnant women to experience unusual sensations during pregnancy. That is because certain hormones are being produced at larger quantities than normal. Sometimes the mother’s pre-existing conditions, whether physical or mental, can be exacerbated during pregnancy.
It’s important for women thinking of getting pregnant to talk with their doctor or a fertility specialist beforehand about existing health problems or concerns. Some medications may be harmful to a fetus and some are harmful to a pregnant woman. It can also be harmful for the woman to stop taking a medication when she is pregnant. Pregnant women or those seeking to become pregnant should follow their doctor’s advice about medications and maintaining or ceasing any type of medical treatment.
Pregnancy complications or problems can be classified as mild or more serious. The serious pregnancy problems require medical attention and management. The mild and annoying ones are generally tolerable, but when in doubt about the extent of the issue, pregnant women should check with their OB-GYN or primary care doctor.
Need help with your pregnancy plans?
We can evaluate existing health concerns before pregnancy or evaluate for infertility issues.
Get in Touch Online
Mild pregnancy complications like constipation, frequent urination & more
Constipation
This is usually caused by hormones early in pregnancy. Pregnant women can help prevent constipation by eating high-fiber foods (whole grains, fruits, vegetables, beans and lentils), exercising regularly, drinking lots of water, and avoiding iron supplements.
Leg cramps
No one is really sure what causes the sharp pain in pregnant women’s calves and feet at night. They can minimize the potential for these sudden pains with gentle leg and ankle movements and prenatal exercise to improve circulation.
Feeling faint
This is typically caused by the brain not getting enough blood or oxygen due to hormone changes. Pregnant women can prevent fainting by standing up from a chair or bed slowly. If a woman feels faint while lying down, she can turn onto her side and not sleep on her back after 28 weeks.
Feeling hot
Again, hormonal changes trigger an increase of blood supply to the skin and make pregnant women sweat more than usual. Pregnant women also may feel hot simply because they have a heater (baby) on board. To combat feeling hot, women can wear loose clothing, keep room temperatures cool, take cooling showers throughout the day, and drink lots of nonalcoholic fluids.
Frequent urination
Often the bane of a pregnant woman’s journey, frequent urination is caused in early pregnancy by progesterone and human chorionic gonadotropin hormones. By the third trimester, pelvic floor muscles relax slightly to prepare for delivery, pressing on the bladder and causing the more frequent need to urinate.
Skin and hair changes
The skin becomes more sensitive during pregnancy. Birthmarks, freckles and nipples tend to darken (but usually fade after the baby is born). The skin burns more easily in the sun. Hair can grow faster and might be greasier. Again, hormones are to blame.
Varicose veins
When veins, especially in the legs or vulva, become swollen during pregnancy, they become uncomfortable but it’s not harmful. To diminish the chance of varicose veins, pregnant women should avoid standing for long periods of time, sitting cross-legged or gaining weight. They should sleep with their legs elevated and exercise to improve their circulation.
Related Reading: How does conception happen?
More serious pregnancy complications like preeclampsia & gestational diabetes
Some symptoms and conditions during pregnancy could pose severe risk to the mother, baby or both. However, with regular prenatal health checks with a healthcare provider, many of these pregnancy complications can be diagnosed early and managed throughout pregnancy. And if a pregnant woman is concerned she may have one of the following issues, she should seek evaluation.
Diabetes
If a woman has pre-existing diabetes that is not under control, she is at risk for multiple pregnancy complications including birth defects, early onset of preeclampsia, visual damage, macrosomia (a newborn much larger than normal) and fetal death.
Preeclampsia
The sudden onset of high blood pressure after the 20th week of pregnancy is a condition known as preeclampsia (pree-ih-KLAMP-see-uh). This disorder causes high blood pressure, swelling, blurred vision, dizziness, headaches and abdominal pain for the mother. It doesn’t uniformly cause all the symptoms or signs. Sometimes only one may be clinically apparent.
Sometimes, preeclampsia can lead to liver or kidney damage, seizure, a stroke or coma for the mother. In addition, preeclampsia reduces blood supply to the fetus, decreasing the delivery of oxygen and nutrients to the growing baby.
The cause of this disorder is not completely understood. Some experts believe it may originate from the abnormal development of new blood vessels, called the placenta, that form to nourish the fetus throughout pregnancy. The cause could also be linked to immune system disorders or genes.
The only treatment for preeclampsia is to deliver the baby. However, if the timing might result in a preterm birth, then the family and provider will need to discuss the potential health risks to the baby and the mother.
This is why it is imperative that a pregnant woman have regular visits with her doctor that always include blood pressure testing. Even after pregnancy, women should continue to be monitored for high blood pressure and related conditions.
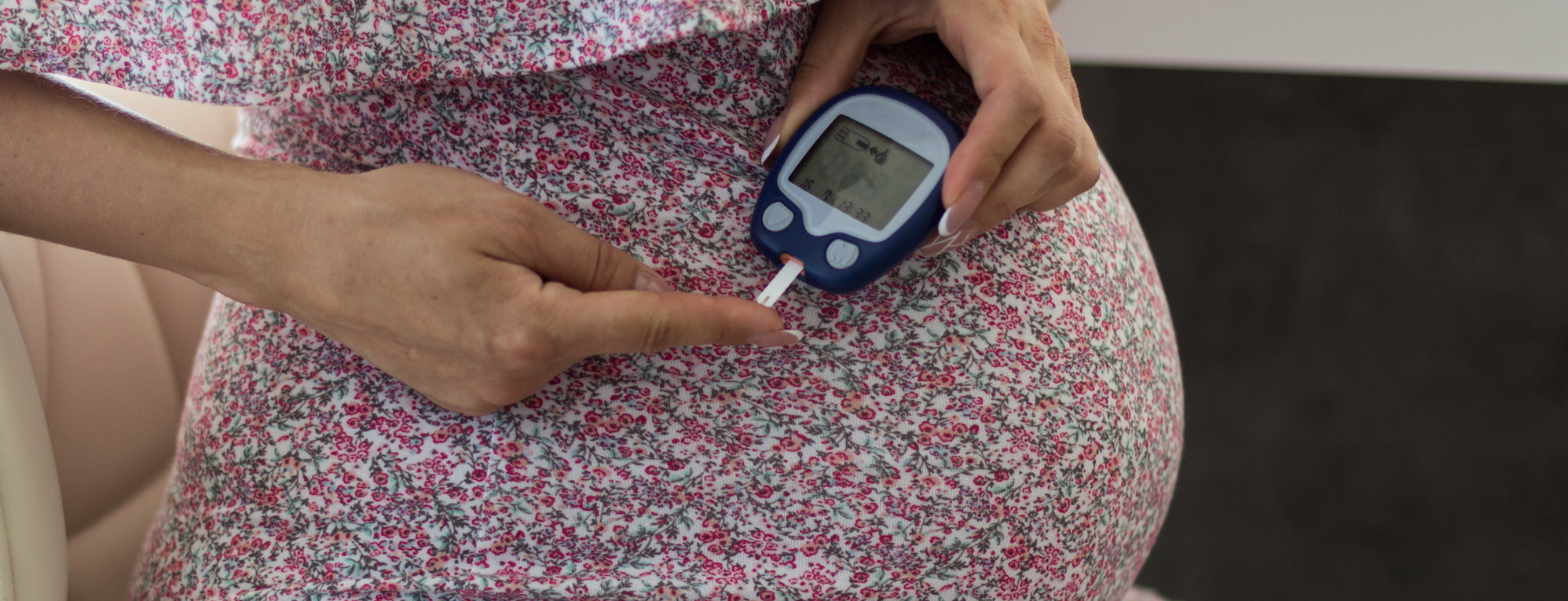
Gestational diabetes
If a pregnant woman’s blood sugar level gets too high, it could trigger gestational diabetes. This condition can affect women who have never had diabetes before becoming pregnant.
Gestational diabetes tends to show up early in the third trimester. Often, there are no symptoms and it can only be detected with regular blood draws. Many providers start testing for this condition between 24 and 28 weeks of pregnancy as part of a regular care plan.
When blood sugar levels are not well controlled, it can lead to problems during pregnancy, such as high blood pressure and preeclampsia. Gestational diabetes can cause a developing baby to grow too much. A too-large baby will force a cesarean section (C-section) delivery or else risk being born with nerve damage.
Gestational diabetes can be managed through eating healthy foods, regular exercise, regular monitoring of blood sugar by a healthcare provider, and taking insulin (if prescribed by a doctor).
Related Reading: Maximize Your Fertility When Trying to Get Pregnant
Bleeding during pregnancy
Early on, bleeding during pregnancy can be common, but if it happens later, it could signal something more serious. No matter when bleeding occurs, a pregnant woman should always call her doctor right away.
In the first trimester, bleeding occurs in about 15% to 25% of women. It can occur in the few weeks after fertilization or as the blood vessels in the cervix and uterus are developing to support the fetus. However, early bleeding during pregnancy could also be caused by infection, miscarriage or ectopic pregnancy.
Bleeding in the first trimester does not necessarily warrant a phone call to the provider. Most bleeding in the first trimester is incidental. If it is a sign of a miscarriage, generally there is nothing a provider can do to prevent it. However, that does not mean the woman cannot call the provider to find out what’s going on.
Into the second and third trimesters, heavy bleeding could indicate the potential of a preterm birth or a complication with the placenta. Problems with the placenta can include its dislocation from the lining of the uterus (known as placental abruption) or the opposite, when it becomes inseparable from the uterine wall (placenta accreta). Both conditions can cause life-threatening blood loss for the mother during delivery.
This is why regular pelvic ultrasound testing during pregnancy is imperative. This in-office imaging test can detect problems with the cervix, uterine lining and placenta that should be addressed by a healthcare provider as early as possible.
Related Reading: Why me? One unexpected journey to get pregnant.
Anxiety and depression during pregnancy
While being pregnant is an exciting time in a woman’s life, it can also be a stressful one. It may be surprising to learn that anxiety and depression during pregnancy is one of the most common complications of pregnancy; it’s not just a postpartum condition.
Hormonal changes, family history, previous signs of depression or anxiety, and temporary changes in brain chemistry can all play a part in causing mental health struggles during pregnancy. In addition, women who suffer problems in pregnancy are more prone to mental health issues than those who don’t have problem pregnancies.
Anxiety and depression during pregnancy can take the forms of intense sadness, feeling helpless or worthless, loss of interest in things the woman likes to do, constant worrying, crying a lot, irritability, changes in eating habits, withdrawing from friends and family, and thoughts of harming herself or the baby.
Mental health challenges during pregnancy can affect both mother and baby. For the mother, feeling low can lead from not eating healthy foods, skipping prenatal care checkups and otherwise not taking wellness seriously.
These challenges can lead to possible thoughts of (or actual) suicide. Effects on the baby can include premature birth, low birth weight, and learning and behavioral problems later in life.
Anxiety and depression during pregnancy can sometimes be treated, but it requires a pregnant woman being honest and open with her care team. Treatments can include therapy, support groups and medication.
Anemia during pregnancy
For a pregnant woman, having enough of the mineral iron in her body is important, as new blood vessels form and an increased amount of blood circulates to support the fetus. Without sufficient iron, a condition called iron deficiency anemia can occur, which means the body is not producing enough red blood cells to carry oxygen in the bloodstream.
Symptoms of anemia include tiredness, feeling weak, irregular heartbeats, shortness of breath, dizziness, pale skin or cold hands and feet.
There are two other types of anemia as well: folate-deficiency anemia and vitamin B-12 deficiency. Folate, a vitamin found in leafy green vegetables, is fundamental to a pregnant woman because it aids the body in producing new, healthy red blood cells. A folate deficiency inhibits production of red blood cells and can cause certain types of birth defects and low birth weight.
The body also needs vitamin B-12 to produce red blood cells. A vitamin B-12 deficiency can be linked to birth defects and preterm birth.
Folic acid supplements are readily available to help maintain folate levels. In addition, a pregnant woman can ward off a B-12 deficiency by eating meat, poultry, dried beans, fortified grains, dairy, eggs and foods high in vitamin C. Always check with a doctor before adding supplements to a diet.
Having problems getting pregnant?
Find out what causes infertility.
Get More Information